Matt Mendes, MD
Director, CO ACEP Board of Directors
Introduction
Refractory ventricular fibrillation (VF) is loosely defined as VF that is unresponsive to epinephrine, 3 defibrillation attempts, and 1 dose of an antidysrhythmic. The classic underlying etiology is a coronary occlusion. These cases are incredibly frustrating as they represent an opportunity to not only obtain return of spontaneous circulation (ROSC) but result in a full neurological recovery. The recent ARREST trial published in Lancet in 2020 was stopped early due to how well the extracorporeal membrane oxygenation (ECMO or ECPR) arm of the study performed against usual care. While ECMO is an exciting and promising therapeutic agent for refractory VF, it is still largely unavailable to the typical emergency physician. Additionally, the evidence surrounding how to treat refractory VF is challenging to interpret. This article will attempt to compile that evidence into a practical algorithm for refractory VF.
The Case
You are notified by EMS that they are emergently transporting a 55-year-old male smoker with a history of hypertension and pre-diabetes who had a witnessed cardiac arrest. They have given 3 doses of epinephrine, 1 dose of amiodarone, and shocked the patient 2 times. They arrive to your ED 10 minutes later and report that the patient was witnessed by family to grab his chest and then go unresponsive at home. CPR was immediately started and 911 was called. The first rhythm for EMS was coarse ventricular fibrillation (VF) and was unresponsive to shocks. EMS reports that since starting transport they have placed an advanced airway with capnography values consistently around 25. EMS also gave another round of epinephrine and amiodarone.
Clinical Course
The initial rhythm check in the emergency room is noted to be coarse VF. The ED physician noted that the prehospital pad placement was anterior-lateral, so they instructed staff to change the pads to the anterior-posterior position. Another shock was unsuccessful so 40mg of esmolol was given IV. Pulses were felt on the next rhythm check and a post-ROSC EKG showed a STEMI in an LAD pattern. The cath lab was activated. The patient was eventually discharged at his baseline neurological function and returned to work 3 months later.
Discussion
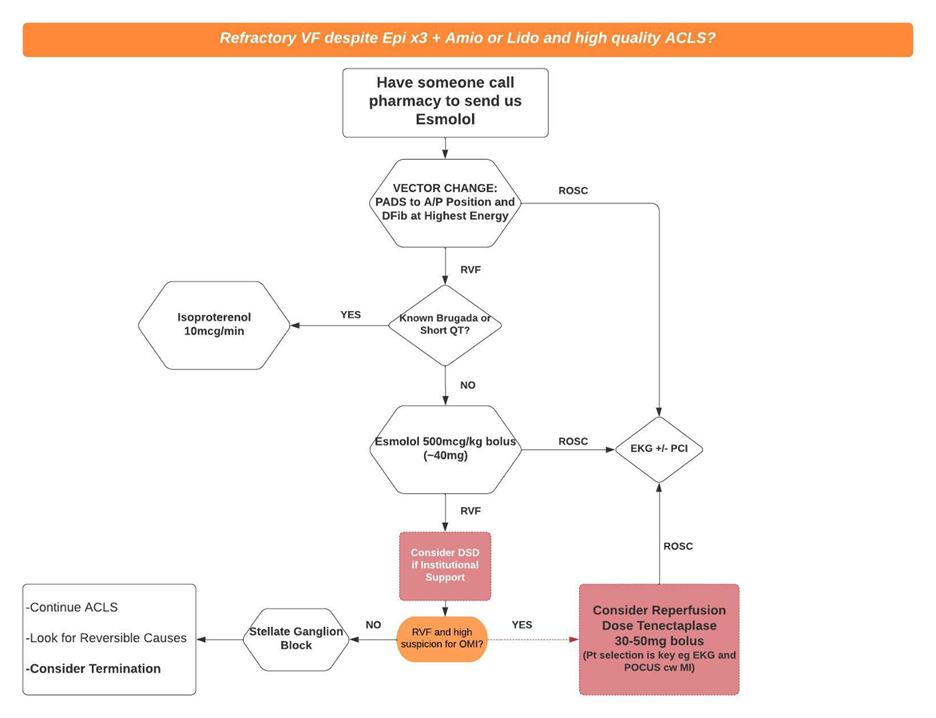
There are many possible therapies posed for refractory VF and unfortunately most have limited evidence at the time of this article. Some of the proposed interventions include percutaneous coronary intervention (PCI), ECMO, esmolol, isoproterenol, dual sequential defibrillation (DSD), vector change defibrillation, thrombolysis, and a stellate ganglion block. In reviewing major resuscitation guidelines, the American Heart Association (AHA) and the European Resuscitation Council (ERC) recommend PCI/ECMO in cases of refractory VF. Esmolol is mentioned favorably by the AHA but not commented on by the ERC. Isoproterenol is recommended by both the AHA and ERC for cases of refractory VF where the patient has known Brugada or short-QT syndrome. The ERC recommends against DSD other than in research settings while the AHA does not make any comments on it. Neither guideline mentions stellate ganglion blocks or vector change defib.
We will briefly review the above interventions and then propose an algorithm for implementing them.
Esmolol is a cardioselective beta-blocker that is thought to protect against the harmful effects of epinephrine (i.e., increased sensitivity of myocardium/decreased arrhythmia threshold). The dose is a 500mcg bolus (~40mg for most adults) followed by an infusion. It has a number needed to treat (NNT) of 3 for sustained ROSC or survival-to-discharge and an NNT of 6 for survival with favorable neurologic function.
Vector change defibrillation is switching the pads from the anterior-lateral position to the anterior-posterior position. This is thought to result in a better vector of electricity through the heart.
DSD can mean two things:
Dual SEQUENTIAL Defibrillation – 2 back-to-back rapid shocks
Dual SIMULTANEOUS Defibrillation – 2 shocks at the same time
It is likely that no one can truly attain dual simultaneous and most studies are using dual sequential protocols. A recent pilot study, the DOSE VF RCT showed in preliminary data that vector change and DSD were not different, but both were better than typical defib. Because of the concern for defibrillator damage, you should only attempt DSD if you have institutional support.
Isoproterenol is a beta agonist recommended by the AHA and ERC for treatment of electrical storm (refractory VF or VT) in patients with Brugada or short QT syndrome because it is thought to stabilize the myocardium by increasing intracellular levels of calcium.
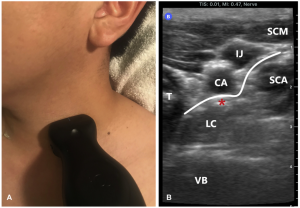
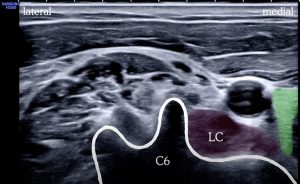
Stellate Ganglion nerve block is done ultrasound-guided on the left side of the neck with 10mL of lidocaine. This is thought to mimic the cardiac sympathetic denervation procedure typically done by way of thoracic surgery.
 Systemic thrombolysis has been proposed as an option for refractory VF in two recent case reports in the American Journal of Emergency Medicine.
Systemic thrombolysis has been proposed as an option for refractory VF in two recent case reports in the American Journal of Emergency Medicine.
Conclusion
The following is a proposed algorithm for ED providers who do not have esmolol immediately available in the code cart:
References
- Al-Khatib SM, Stevenson WG, Ackerman MJ, et al. 2017 AHA/ACC/HRS Guideline for Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: Executive Summary. Vol 138.; 2018. doi:10.1161/CIR.0000000000000548
- Alm-Kruse K, Sørensen G, Osbakk SA, et al. Outcome in refractory out-of-hospital cardiac arrest before and after implementation of an ECPR protocol. Resuscitation. 2021;162(September 2020):35-42. doi:10.1016/j.resuscitation.2021.01.038
- As A, With C, For L, Fibrillation SV. FOR SHOCK-RESISTANT VENTRICULAR FIBRILLATION A M I O DA R O N E V E R S U S L I D O C A I N E F O R S H O C K- R E S I STA N T V E N T R I C U L A R F I B R I L AT I O N. 2002;346(12):884-890.
- Association AH. Highlights of the 2019 Focused Updates to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. doi:10.1080/00913847.1996.11440054
- Bell SM, Lam DH, Kearney K, Hira RS. Management of Refractory Ventricular Fibrillation (Prehospital and Emergency Department). Cardiol Clin. 2018;36(3):395-408. doi:10.1016/j.ccl.2018.03.007
- Böttiger BW, Arntz H-R, Chamberlain DA, et al. Thrombolysis during Resuscitation for Out-of-Hospital Cardiac Arrest. N Engl J Med. 2008;359(25):2651-2662. doi:10.1056/nejmoa070570
- Cheskes S, Dorian P, Feldman M, et al. Double sequential external defibrillation for refractory ventricular fibrillation: The DOSE VF pilot randomized controlled trial. Resuscitation. 2020;150(February 2020):178-184. doi:10.1016/j.resuscitation.2020.02.010
- Deakin CD, Morley P, Soar J, Drennan IR. Double (dual) sequential defibrillation for refractory ventricular fibrillation cardiac arrest: A systematic review. Resuscitation. 2020;155(June 2020):24-31. doi:10.1016/j.resuscitation.2020.06.008
- Driver BE, Debaty G, Plummer DW, Smith SW. Use of esmolol after failure of standard cardiopulmonary resuscitation to treat patients with refractory ventricular fibrillation. Resuscitation. 2014;85(10):1337-1341. doi:10.1016/j.resuscitation.2014.06.032
- Dyer S, Mogni B, Gottlieb M. Electrical storm: A focused review for the emergency physician. Am J Emerg Med. 2020;38(7):1481-1487. doi:10.1016/j.ajem.2020.04.017
- Gottlieb M, Dyer S, Peksa GD. Beta-blockade for the treatment of cardiac arrest due to ventricular fibrillation or pulseless ventricular tachycardia: A systematic review and meta-analysis. Resuscitation. 2020;146(July):118-125. doi:10.1016/j.resuscitation.2019.11.019
- Hamera JA, Bryant NB, Shievitz MS, Berger DA. Systemic thrombolysis for refractory cardiac arrest due to presumed myocardial infarction. Am J Emerg Med. 2021;40:226.e3-226.e5. doi:10.1016/j.ajem.2020.07.053
- Lee YH, Lee KJ, Min YH, et al. Refractory ventricular fibrillation treated with esmolol. Resuscitation. 2016;107:150-155. doi:10.1016/j.resuscitation.2016.07.243
- Long DA, Long B, April MD. Does β-Blockade for Treatment of Refractory Ventricular Fibrillation or Pulseless Ventricular Tachycardia Improve Outcomes? Ann Emerg Med. 2020;76(1):42-45. doi:10.1016/j.annemergmed.2020.01.025
- Margus C, Correa A, Cheung W, et al. Stellate Ganglion Nerve Block by Point-of-Care Ultrasonography for Treatment of Refractory Infarction-Induced Ventricular Fibrillation. Ann Emerg Med. 2020;75(2):257-260. doi:10.1016/j.annemergmed.2019.07.026
- Miraglia D, Miguel LA, Alonso W. Esmolol in the management of pre-hospital refractory ventricular fibrillation: A systematic review and meta-analysis. Am J Emerg Med. 2020;38(9):1921-1934. doi:10.1016/j.ajem.2020.05.083
- Miraglia D, Miguel LA, Alonso W. Double Defibrillation for Refractory In- and Out-of-Hospital Cardiac Arrest: A Systematic Review and Meta-Analysis. J Emerg Med. 2020;59(4):521-541. doi:10.1016/j.jemermed.2020.06.024
- Miraglia D, Miguel LA, Alonso W. The evolving role of novel treatment techniques in the management of patients with refractory VF/pVT out-of-hospital cardiac arrest. Am J Emerg Med. 2020;38(3):648-654. doi:10.1016/j.ajem.2019.11.003
- Miraglia D, Ramzy M. Double external defibrillation for shock-refractory ventricular fibrillation cardiac arrest: A step towards standardization. Am J Emerg Med. 2021;41:73-79. doi:10.1016/j.ajem.2020.12.031
- Priori SG, Blomstrom-Lundqvist C, Mazzanti A, et al. 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death the Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the Europea. Eur Heart J. 2015;36(41):2793-2867l. doi:10.1093/eurheartj/ehv316
- Reyner K, Heffner AC, Garvey JL, Tayal VS. Successful use of intra-arrest thrombolysis for electrical storm due to acute myocardial infarction. Am J Emerg Med. 2015;33(7):990.e5-990.e8. doi:10.1016/j.ajem.2014.12.050
- Soar J, Böttiger BW, Carli P, et al. European Resuscitation Council Guidelines 2021: Adult advanced life support. Resuscitation. 2021;161:115-151. doi:10.1016/j.resuscitation.2021.02.010
- Yannopoulos D, Bartos J, Raveendran G, et al. Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): a phase 2, single centre, open-label, randomised controlled trial. Lancet. 2020;396(10265):1807-1816. doi:10.1016/S0140-6736(20)32338-2